Table of Contents
Overview – Skin Structure
The skin is the body’s largest organ and serves as a complex barrier and interface with the environment. Understanding skin structure is vital for final-year medical students as it underpins the pathophysiology of a wide range of dermatological conditions. This page will break down the key anatomical layers—epidermis, dermis, and hypodermis—along with their cellular components and functional roles. The topic “skin structure” is foundational for clinical dermatology and is essential knowledge for exams and practice.
Functions of Normal Skin
- Protective barrier (mechanical and chemical)
- Prevents fluid loss (via intercellular lipids and overlapping cells)
- Immune defense against microorganisms
- Immunological barrier (Langerhans cells)
- Endocrine function (Vitamin D synthesis via UV exposure)
- Vitamin D → ↑ Calcium absorption (gut) and ↑ renal calcium retention
- Melanin production (UV protection)
- Thermoregulation via blood flow control
- Sensory organ for touch, pain, temperature
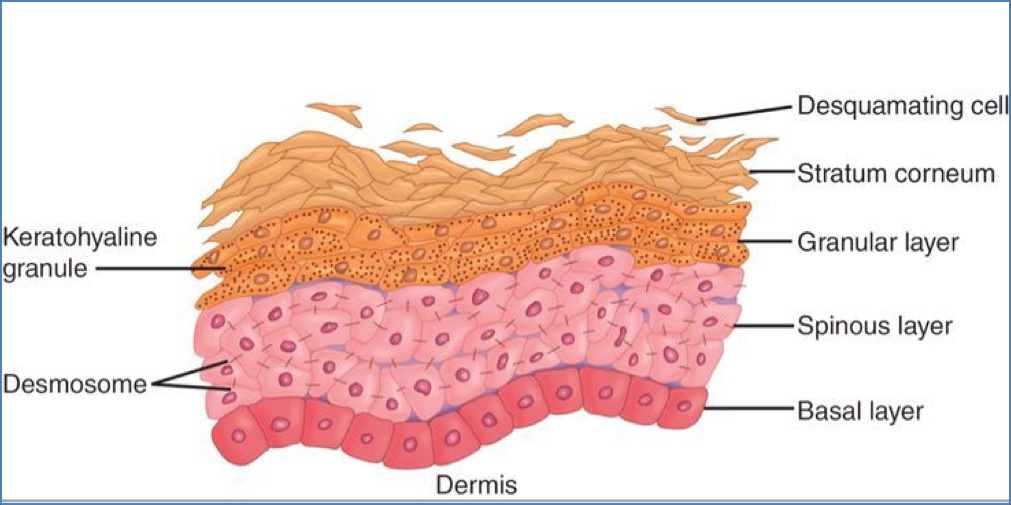
Epidermis
- Stratified squamous keratinised epithelium
- Avascular and primarily cellular (~95% keratinocytes)
- Protective, renewable barrier (0.1–1 mm thick)
Layers (from deep to superficial):
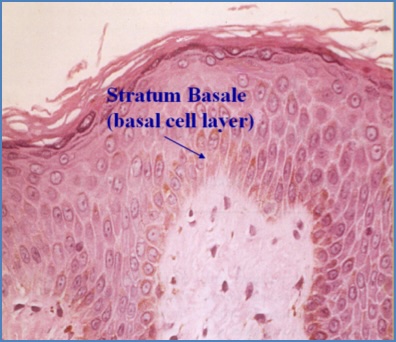
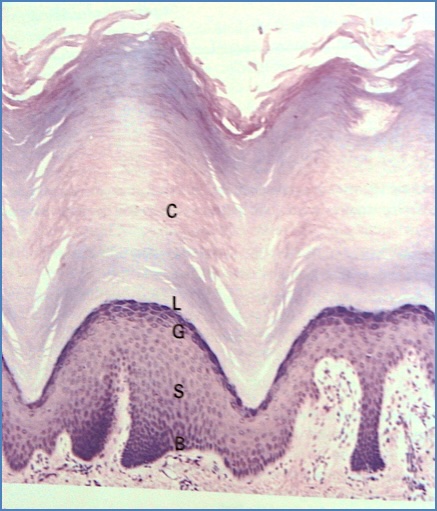
- 1. Stratum Basale (Germinativum):
- Single layer of cuboidal/columnar cells
- Stem cells divide and differentiate into keratinocytes over ~14 days
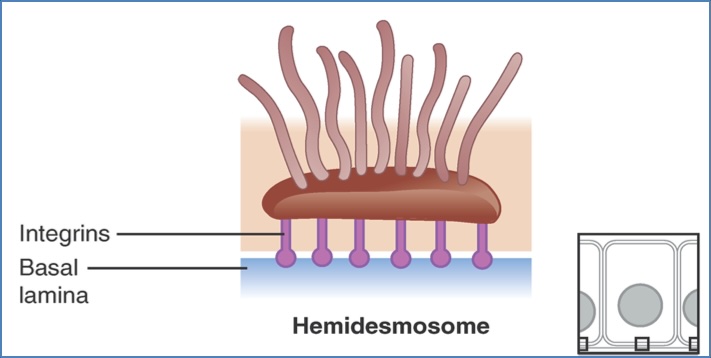
- Attached to basement membrane via hemidesmosomes
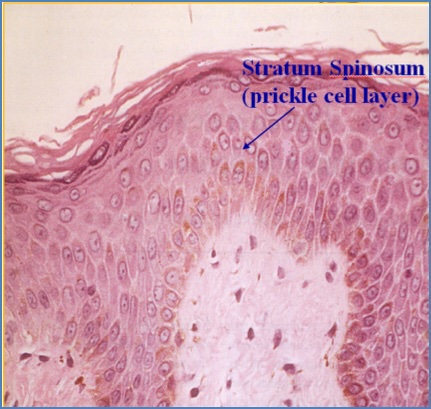
- 2. Stratum Spinosum (Prickle cell layer):
- Several layers of polyhedral keratinocytes
- Tonofibrils attach to desmosomes
- Contains Langerhans cells (APCs)
- Lamellar bodies → extracellular lipid barrier
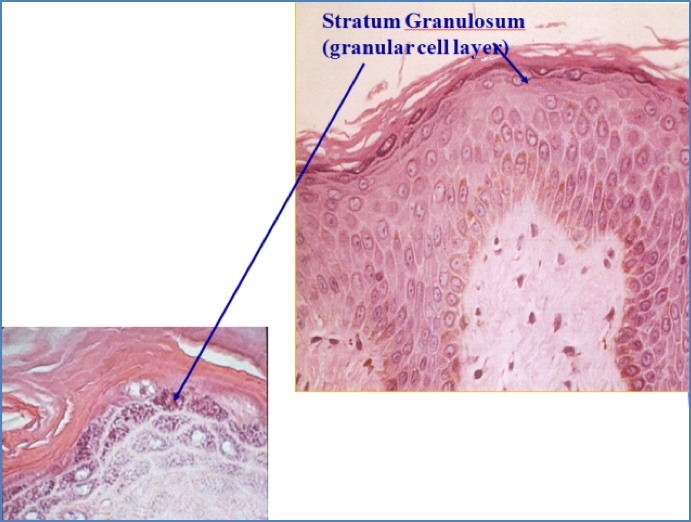
- 3. Stratum Granulosum:
- 3–5 layers of flattened keratinocytes
- Loss of nuclei
- Keratohyalin granules (profilaggrin, keratin, loricrin)
- Lamellar bodies secrete lipid-rich “mortar” between cells
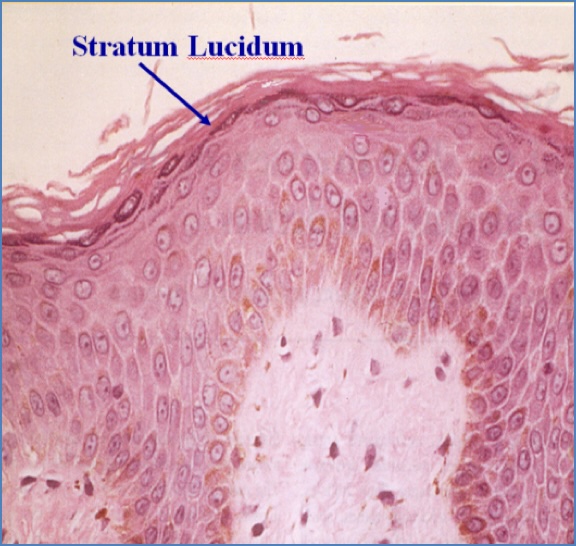
- 4. Stratum Lucidum:
- Only in thick, glabrous skin (palms/soles)
- Flattened, anucleate cells
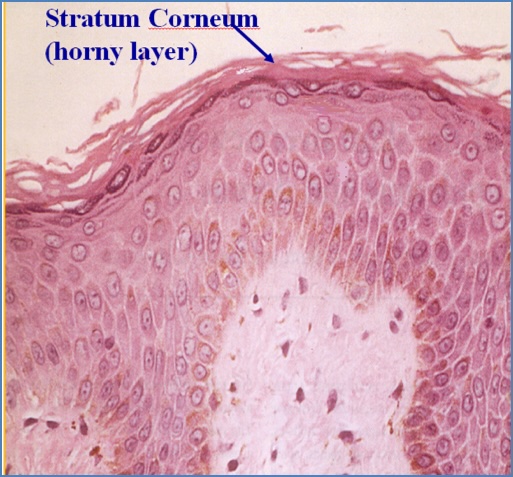
- 5. Stratum Corneum:
- 5–50 layers of dead, flattened squames
- No nuclei or organelles
- Keratin and lipids create a strong moisture-retaining barrier
- Thickest in glabrous skin
Epidermal Cells:
- Keratinocytes:
- Produce keratin (types I & II → form tonofilaments)
- Connected by desmosomes (cell-cell) and hemidesmosomes (cell-BM)
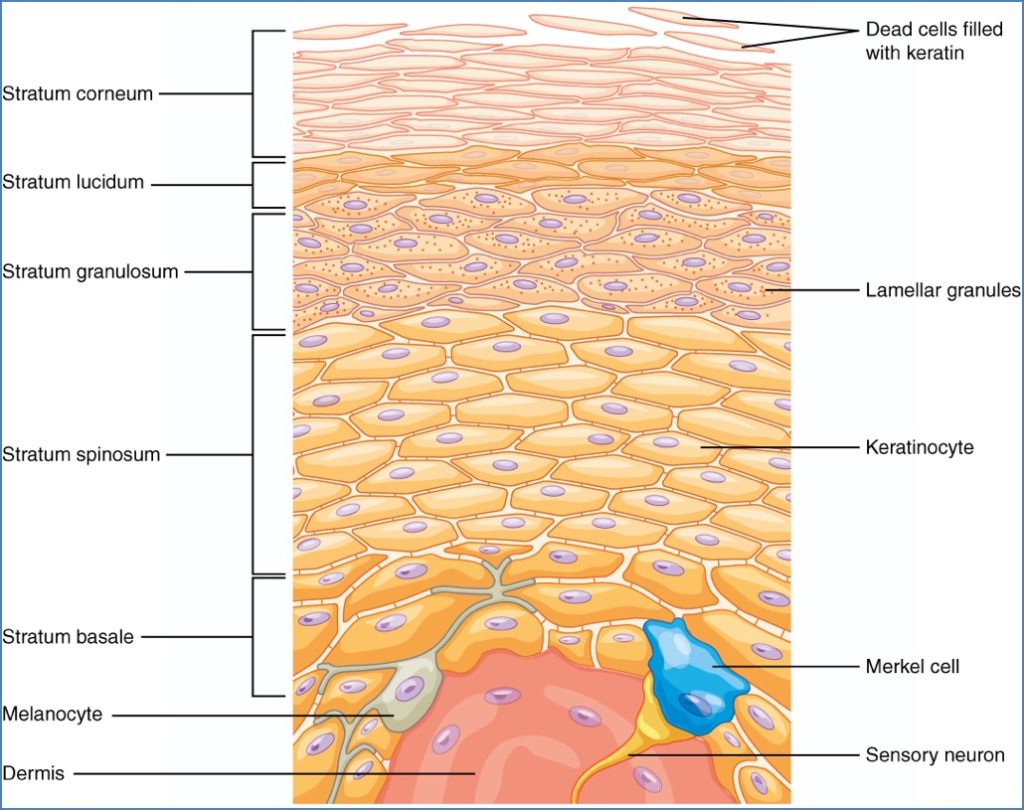
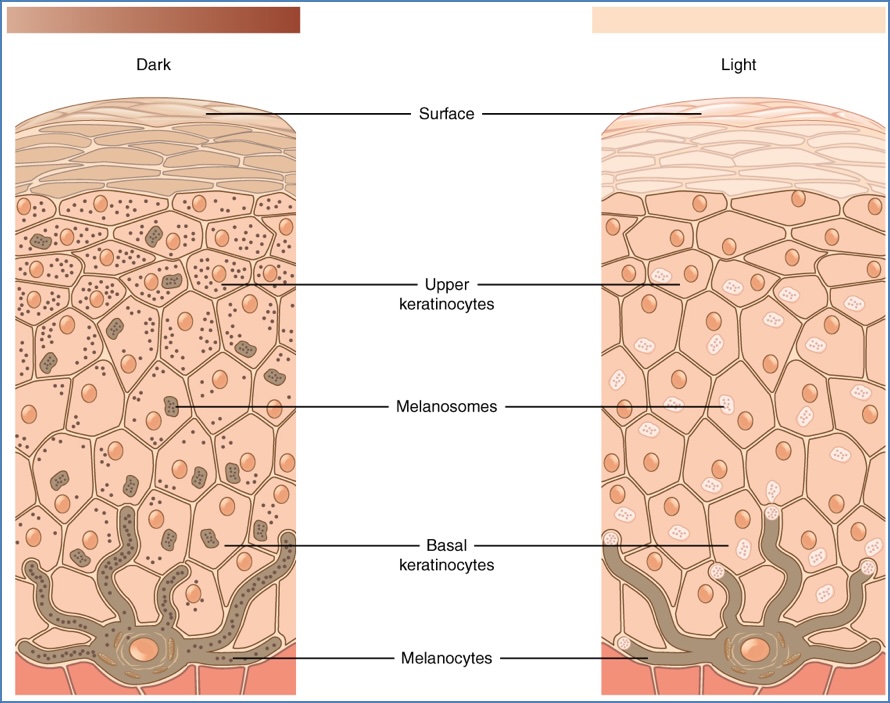
- Melanocytes:
- Found in basal layer, dermis, and hair follicles
- Produce melanin in melanosomes → transferred to keratinocytes
- Racial pigmentation depends on activity, not number

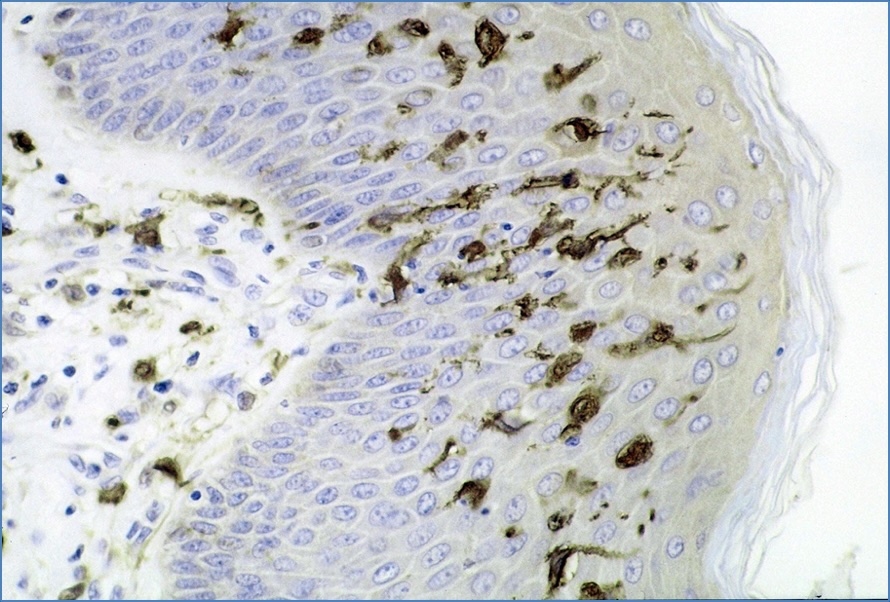
- Langerhans Cells:
- APCs with dendritic processes in stratum spinosum
- Migrate to lymph nodes for immune surveillance
- Merkel Cells:
- Sensory mechanoreceptors
- Contain catecholamine granules; neuroendocrine function
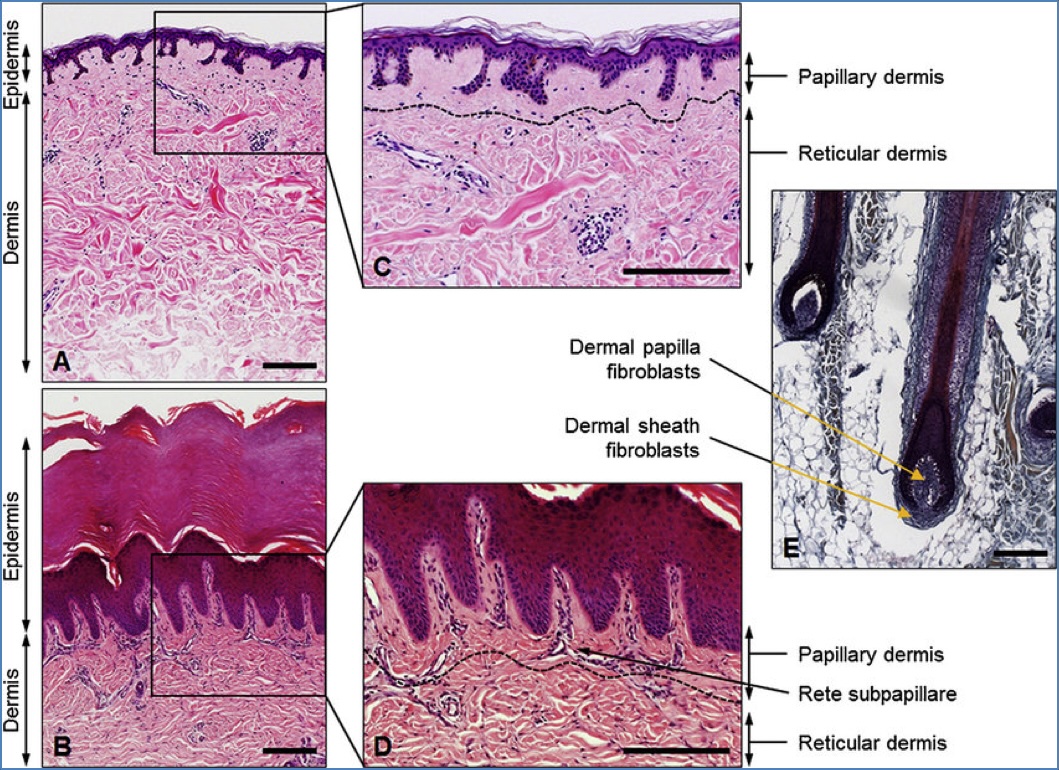
Dermal-Epidermal Junction
- Interface between epidermis (stratum basale) and dermis
- Components:
- Basement membrane: Lamina lucida (anchors hemidesmosomes) + lamina densa (type IV collagen)
- Hemidesmosomes: Link keratin tonofilaments to BM
- Rete ridges & dermal papillae: Strengthen epidermal-dermal adhesion
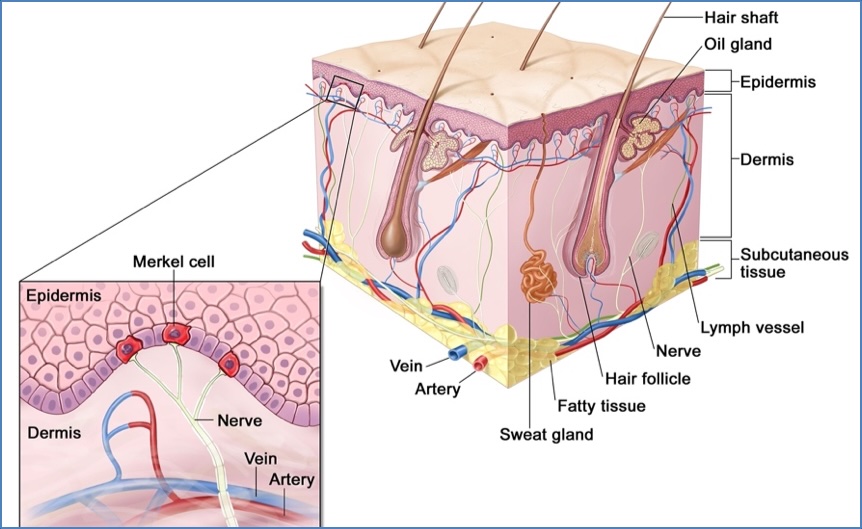
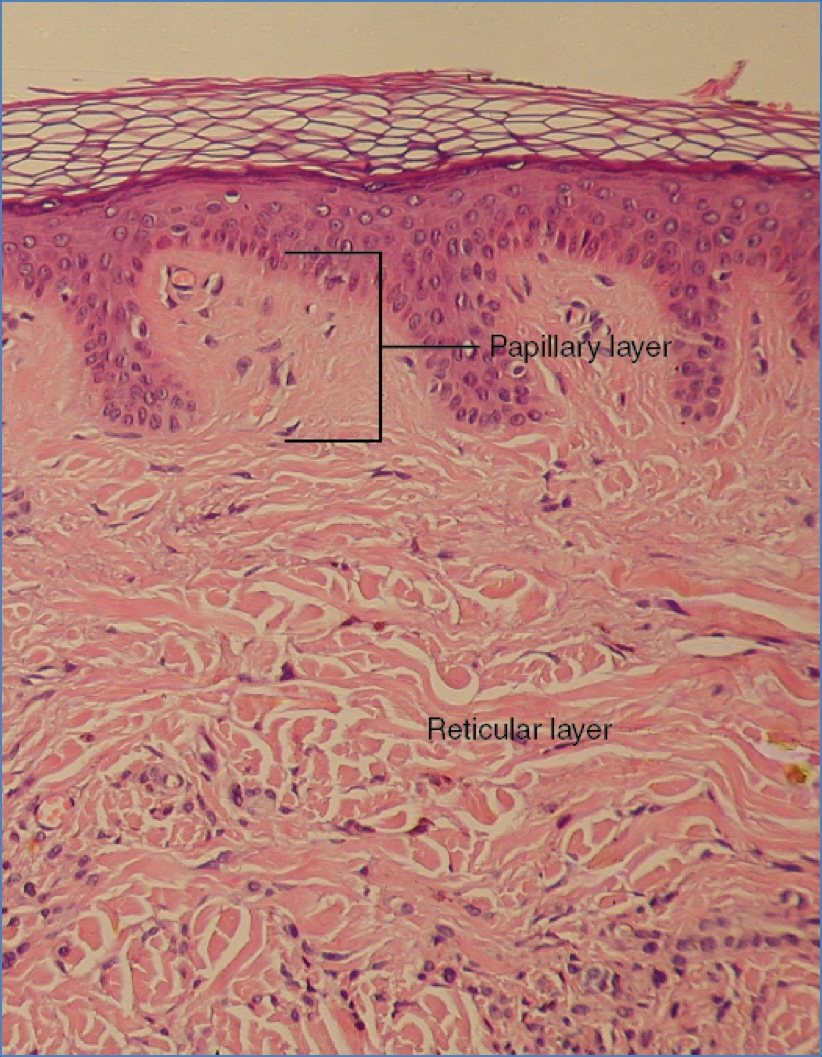
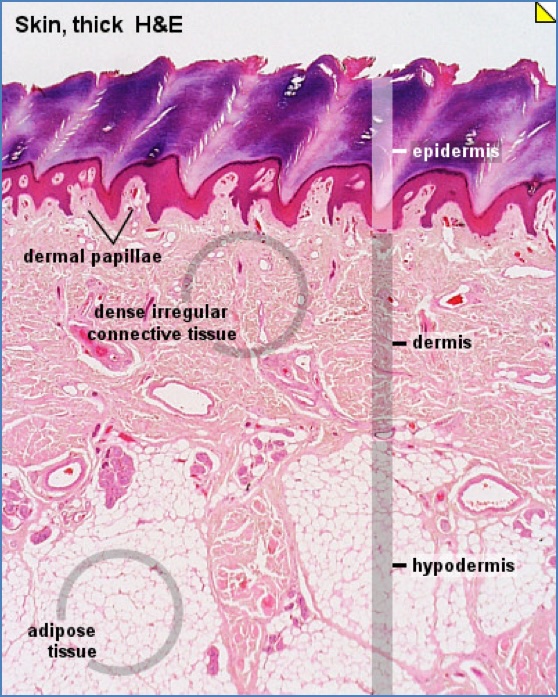
Dermis
- Mainly extracellular matrix (collagen, elastin, GAGs)
- Two layers:
- Papillary layer (superficial): Fine collagen
- Reticular layer (deep): Thick collagen, stronger
- Contains:
- Fibroblasts (collagen/elastin synthesis)
- Histiocytes (phagocytic macrophages)
- Mast cells (histamine → allergies)
- Lymphocytes (perivascular)
- Blood vessels, nerves
- Skin appendages (hair follicles, sweat glands, arrector pili)
Hypodermis
- Also called subcutaneous tissue
- Mostly adipose tissue
- Functions:
- Thermal insulation
- Energy storage
- Contains blood vessels and nerves

Epidermopoiesis & Desquamation
Epidermopoiesis (Renewal)
- Continuous regeneration from basal cells
- Driven by growth factors (EGF, TGFa, FGF)
- Full turnover: ~6 weeks (14 days to corneum, 14 to shed)
Desquamation (Shedding)
- Degradation of desmosomes (e.g. by cholesterol sulfatase)
- Balance with cell production maintains skin homeostasis
Summary – Skin Structure
Understanding skin structure is essential for interpreting dermatological pathology and appreciating the complexity of skin function. This high-yield breakdown covered all layers of the skin—epidermis, dermis, and hypodermis—with emphasis on their cells, architecture, and physiological roles. The “skin structure” knowledge underpins clinical approaches in dermatology, especially in conditions affecting specific layers or cellular components. For a broader context, see our Skin & Dermatology Overview page.